Healthcare Compliance Perspective:
Kickbacks paid to referral sources and/or Medicare beneficiaries result in false claims.
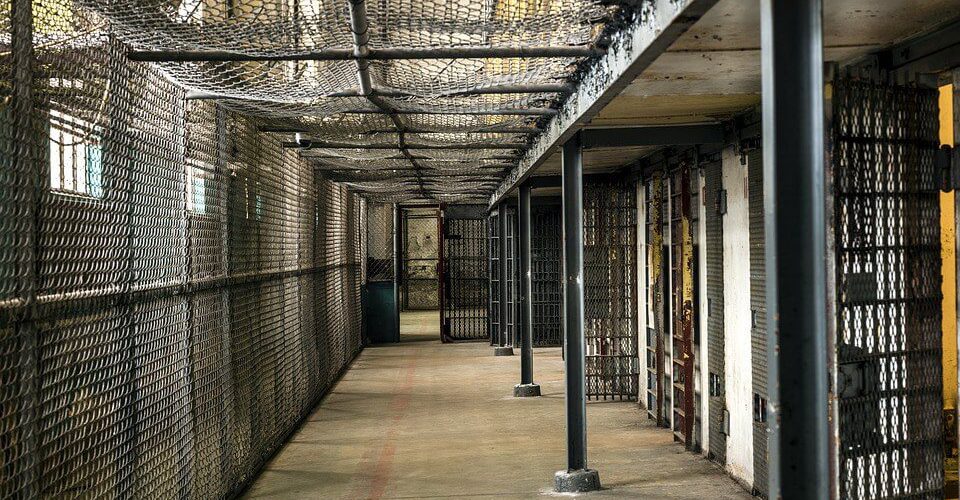
The owner and operator of five home health agencies was sentenced by a U.S. District Court Judge to 480 months in prison last week. This stiff sentence was given as a consequence for the agencies’ owners conspiring to defraud Medicare & Medicaid programs of more than $17 million, plus laundering the money he stole. The two Medicaid programs involved are known as the Medicaid-funded Home and Community-Based Service (HCBS) and Primary Home Care (PHC) Programs. These two programs are more commonly known as “provider attendant services” (PAS) and this case marks the largest PAS fraud case charged in state history.
The man pleaded guilty last March to two counts of conspiracy to commit healthcare fraud and one count of conspiracy to launder monetary instruments.
The man along with his co-defendant daughter and other family members paid Medicaid patients by cash, check, Western Union and MoneyGram for receiving services from his family’s home health agencies in exchange for the ability to use their Medicare and Medicaid numbers to bill the programs for home healthcare and PAS services. The man and his daughter also paid some of the patients for recruiting other Medicare and Medicaid patients to their agencies. Additionally, they paid kickbacks they termed co-payments to physicians for referring and certifying Medicare and Medicaid patients for home health and PAS services.
The total of the fraudulent claims submitted by the owner of these five home health agencies and his co-conspirators was nearly $18 million; and, of those claims submitted, they received more than $16 million.